 Dr. John Tarbell serves as the CUNY and Wallace Coulter Distinguished Professor of Biomedical Engineering at the Grove School of Engineering. Dr. Tarbell was recently honored for his research with a Special Issue of the journal “Cardiovascular Engineering and Technology” celebrating his 45 years of research in the field. The papers in the special issue represent contributions from his different research areas and his collaborations with students and colleagues. For more details (names, references) refer to https://doi.org/10.1007/s13239-020-00516-5. Below is an edited version of a recent interview with Dr. Tarbell conducted by Dr. Claude Brathwaite from the Grove School of Engineering, Office of Academic Affairs.
Dr. John Tarbell serves as the CUNY and Wallace Coulter Distinguished Professor of Biomedical Engineering at the Grove School of Engineering. Dr. Tarbell was recently honored for his research with a Special Issue of the journal “Cardiovascular Engineering and Technology” celebrating his 45 years of research in the field. The papers in the special issue represent contributions from his different research areas and his collaborations with students and colleagues. For more details (names, references) refer to https://doi.org/10.1007/s13239-020-00516-5. Below is an edited version of a recent interview with Dr. Tarbell conducted by Dr. Claude Brathwaite from the Grove School of Engineering, Office of Academic Affairs.
Early Start
When I started out Biomedical Engineering was not a well-developed discipline. In the 1970s there were only a few BME departments. Unaware of the existence of BME, I obtained undergraduate (Rutgers Univ.) and graduate (Univ. of Delaware) degrees in Chemical Engineering which provided a solid foundation for Biomedical Engineering. As it turned out, my chemical engineering background in Fluid Mechanics and Mass Transfer were highly relevant to understanding blood flow and the physiology of the cardiovascular system.
The Transition
In my transition from chemical engineering to biomedical engineering one early paper describing the possible role of fluid mechanics and mass transport in vascular disease was eye opening (Caro et al. Proc R Soc Lond B Biol Sci. 1971). Shortly after reading that paper I obtained my first major faculty position, again in chemical engineering, at Penn State University. There I pursued biomedical engineering studies of the cardiovascular system with the encouragement of my new colleague, James Ultman. I realized early on that I had a background in organic and physical chemistry, but not biochemistry. I had not formally studied biology, physiology, molecular biology or cell biology – all part of modern BME training. I had to learn these subjects along the way as necessary to solve the research problems I was pursuing. This was Problem Based Learning, a truly exciting way to learn.
On Problem Based Learning
Text book problems are one thing, more open ended problems are another. In engineering education there has been a far-reaching effort to introduce Problem Based Learning (PBL) through problems that do not have a unique solution. I have introduced PBL in my own courses, my colleagues have done the same. Many universities have developed entire courses based on Problem Based Learning.
The journey over 45 years – the theme of fluid flow forces on cells
Atherosclerosis– I started my research journey trying to understand the role of blood flow fluid mechanics in atherosclerosis, the disease that underlies heart attacks, strokes and other cardiovascular diseases. I was intrigued by the observation that although you may have high cholesterol concentration in your systemic blood, a primary risk factor for atherosclerosis, you do not have atherosclerosis throughout your cardiovascular system. Only certain blood vessels such as coronary and carotid arteries are highly susceptible to atherosclerosis. The association of altered or disturbed blood flow patterns with these areas of localized of atherosclerosis drove my early interest in this area. In the beginning we thought fluid flow effects on mass transport of cholesterol from blood to the artery wall was critical, and I investigated this hypothesis for several years.
Mechanobiology – Then we realized that the mechanical forces of blood flow on the artery wall, particularly shear stress, altered the biochemical behavior of the vessel lining cells (endothelial cells) by a mechanism called mechano-transduction — the conversion of a mechanical force into a biochemical response in the cell. Mechanotransduction could lead to localized production of biochemicals that enhance the permeability of the vessel wall to cholesterol, leading to localized plaque buildup.
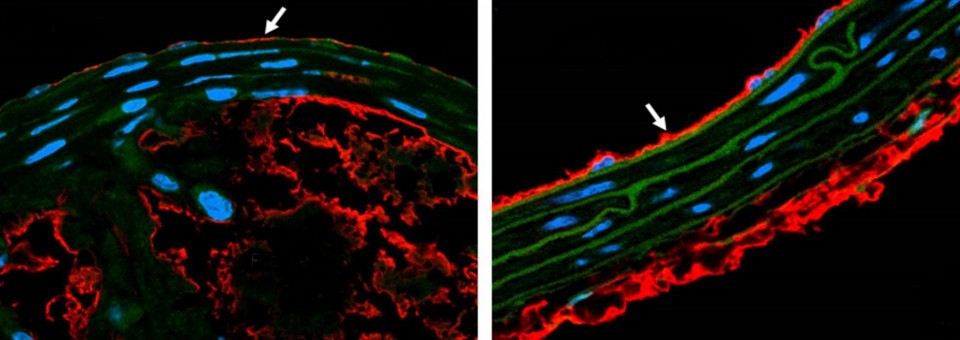
The Glycocalyx – Eventually we turned our attention to the surface layer of proteoglycans (proteins with long sugar molecules attached) that cover endothelial cells and come in direct contact with flowing blood – the so called “glycocalyx”. We hypothesized that the long sugar molecules in the glycocalyx could serve as mechano-sensors for the shear stress of blood flow and transmit the force through the protein backbone to the cell, much like the leaves and branches of a tree sense the force of the wind and use the trunk of the tree to transmit the force to the ground. In my first excursion into this area, we discovered that certain proteoglycans in the glycocalyx were responsible for the shear dependent production of nitric oxide. Nitric oxide is an important vasodilator molecule responsible for flow mediated vasodilation — a sign of healthy vasculature. The glycocalyx also protects blood vessels from inflammation and from becoming leaky to cholesterol carrying proteins. The broader field of glycocalyx research has grown rapidly in recent years with the importance of the glycocalyx receiving increasing recognition.
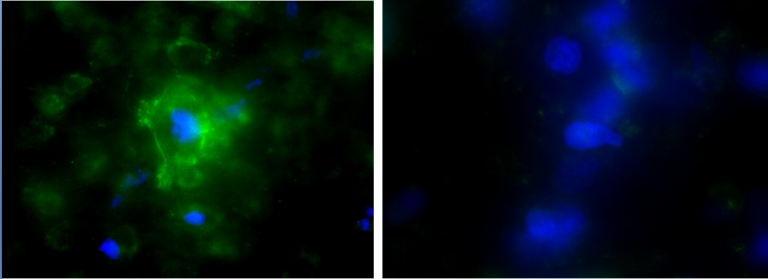
The glycocalyx and Cancer Biology – Back in the early 90s we demonstrated that interstitial flow (flow from high pressure blood vessels into low pressure tissue) on cells within the blood vessel wall (smooth muscle cells) increased their ability to move through the tissue. Subsequently I became aware that cancer tumors tend to be nourished by leaky blood vessels and I hypothesized that they would have an elevated interstitial flow imposing shear stress on cancer cells. We observed in experiments using cancer cells in culture that elevated interstitial flow made cancer cells more motile, suggesting this might contribute to metastasis (the movement of cancer cells from the primary tumor to distant sites). We also discovered that removing the cancer cell glycocalyx reduced cell motility suggesting this might suppress metastasis. This led to experiments in mice showing that renal carcinoma metastasis could be reduced by 95% after selective removal of the glycocalyx.
Infectious Disease – Several very recent studies have shown that the glycocalyx is a protective layer on cells that helps prevent viruses from invading host cells. This is certainly true in the case of COVID-19 that attacks lung epithelial cells and endothelial cells leading to familiar acute symptoms and in too many cases death. The glycocalyx is becoming more widely recognized as a potential target for therapeutics to protect against COVID 19 and other viral and bacterial infections.
The Artificial Heart – While at Penn State University I had the unique opportunity to work with a well-established group that was developing an artificial heart. I founded an Artificial Heart Fluid Mechanics lab that elucidated the fluid flow and shear stress characteristics of artificial hearts and ventricular assist devices under development. Our goal was to generate designs that would minimize blood cell damage and the formation of blood clots. Ventricular assist devices are currently in clinical use while total artificial hearts have limited FDA approval. My last post doctoral fellow at Penn State, Keefe Manning, now a professor in BME, continues to run the Artificial Heart Fluid Mechanics Lab.
Coming to City College and building a Biomedical Engineering Department
After many years at Penn State, I was searching for new opportunities. Fortuitously, a new BME department was forming at City College at that time (2002). I was impressed by the diversity of City College which for me was very welcoming. Distinguished Professor Sheldon Weinbaum, whom I had known for many years through research, was leading the development of the new department, and Morton Denn, one of my professors and mentors at the University of Delaware was there as the Einstein Professor. I saw the opportunity to build a new department in a city with many of the nation’s leading medical institutions that was clearly lacking adequate biomedical engineering infrastructure. I spent 9 years as the first permanent chair of BME during which time we received our first ABET accreditation, greatly expanded our faculty in core areas, increased our research productivity while providing many new opportunities for undergraduate research, and built our national reputation.
Advice to undergraduates
I still remember my first archival publication that was based on my undergraduate research. That was the beginning of my interest in research and my enthusiasm has not waned over 45 years. I pursued many areas of research in the early days before discovering cardiovascular engineering. It took quite a while to find my passion, but when I look back, I can’t imagine a more exciting journey.
Undergraduates who are reading this piece are not likely to be pursuing cardiovascular engineering – that was my path. Your path most likely remains to be discovered. My simple advice to you is to pursue as many opportunities for experience as you can manage. Just focusing on coursework is not the way to go. Stretch yourself and you will be rewarded.